A prosthetic heart valve is an artificial one-way valve surgically implanted into the patient’s heart to replace a missing valve. Typically, an artificial heart valve consists of a diaphragm or a single chamber that is filled with a solution or gel.
Other varieties of this type of heart valve can include those that are fashioned from silicon, plastic, and metal. Prosthetic heart valves may be made of silicone, neoprene, polymyxin, or other material such as a sponge or bladder.
Generally, these devices are considered safer than biological heart valves since they can move water out of the heart chamber through a valve stem rather than via the blood supply. Additionally, they do not require any real surgical procedure in order to place or remove them from the heart.
Besides the convenience of a non-surgical alternative, there are many other reasons why individuals who desire a mechanical valve replacement choose to have prosthetic heart valves instead.
They include higher reliability, reduced costs, simplified exercise requirements, and less discomfort and recovery time, and improved function. These factors make prosthetic heart valves more popular with patients and doctors alike.
However, as with all surgeries, certain risks exist and complications can arise if the surgery is performed incorrectly, including infection, blood clots, complications from anesthesia, or excessive bleeding. Additionally, some of these complications occur more frequently in women than in men.
Depending on the type of prosthetic heart valves being used, their installation usually requires minimally invasive surgery. The location and size of the implant generally determines how much of the anatomy has to be removed and the types of incisions that will be required.
Two types of incision procedures are typically used to insert the devices. One involves the use of an incision similar to a standard Easter ligation where only a small portion of the vas deferens is removed.
The second type of procedure is referred to as a citation-needed procedure, wherein additional tissue is cut away from the breastbone and the endoscope is inserted through tiny cuts into the side of the penis.
Patients undergoing a transcatheter implantation typically experience one or more of the following: a reduction of symptoms, better blood flow, relief from pain and discomfort, decreased cardiac morbidity, improvement in heart function, fewer cardiovascular problems, and a decreased risk of stroke.
This last benefit is desirable, as stroke is one of the leading causes of death among men. This benefit may be even more desirable if their condition is mild, such as milder obesity, mild hypertension, or mild heart disease.
Also, if an individual suffers from chronic conditions or heart disease, the prosthetic heart valve replacement procedure may be a little more complicated and be covered by Medicare.
As mentioned above, a major benefit of the surgery is that it eliminates the need for the patient to undergo a new prosthetic heart valve or surgical procedure. Another benefit is that surgical synthetic valves do not suffer from the same drawbacks that are often associated with natural heart valves (e.g. blockages and Regurgitation).
Therefore, synthetic valves provide patients with a more durable and reliable way to manage their cardiovascular systems. They may also improve patients’ satisfaction with their heart surgeries as well.
Regurgitation is known to be one of the most common complications of ECD (endocardial contraindication) in which the scar created during surgery weakens or blocks the flow of blood to the heart.
With technological advancements, cardiac devices such as the mechanical heart valve replacement, such as those manufactured by Cardiology, Inc. and Medtronic, have come a long way in preventing and stopping the majority of the heart attacks and related complications that occur each year.

For instance, some of the leading causes of death within the U.S. are heart failure, congenital heart disease, ventricular fibrillation, myocardial infarction, strangulation and reattachment, congenital heart defects, and acute cardiac arrest. Most of these complications can be prevented or delayed with the use of an ECD and/or mechanical heart valve replacement.
Moreover, as new and improved prosthetic heart valves are developed and tested by Cardiology, Inc. and other leading cardiovascular device manufacturers, more people will experience the potential benefits and advantages provided by the use of an ECD and/or mechanical valve.
A variety of prosthetic heart valves exist to repair or replace defective heart tissue. While some of these procedures can be very complicated, such as those using traditional ligation, balloon catheterization, or endomyema, others can be performed quickly and easily using mechanical or homograft tissue valves (which require less invasive surgery).
Moreover, while these surgical techniques have proven successful, the procedure can be extremely expensive. By contrast, many patients can now safely undergo mechanical valves as part of their routine medical care without incurring additional surgical costs.
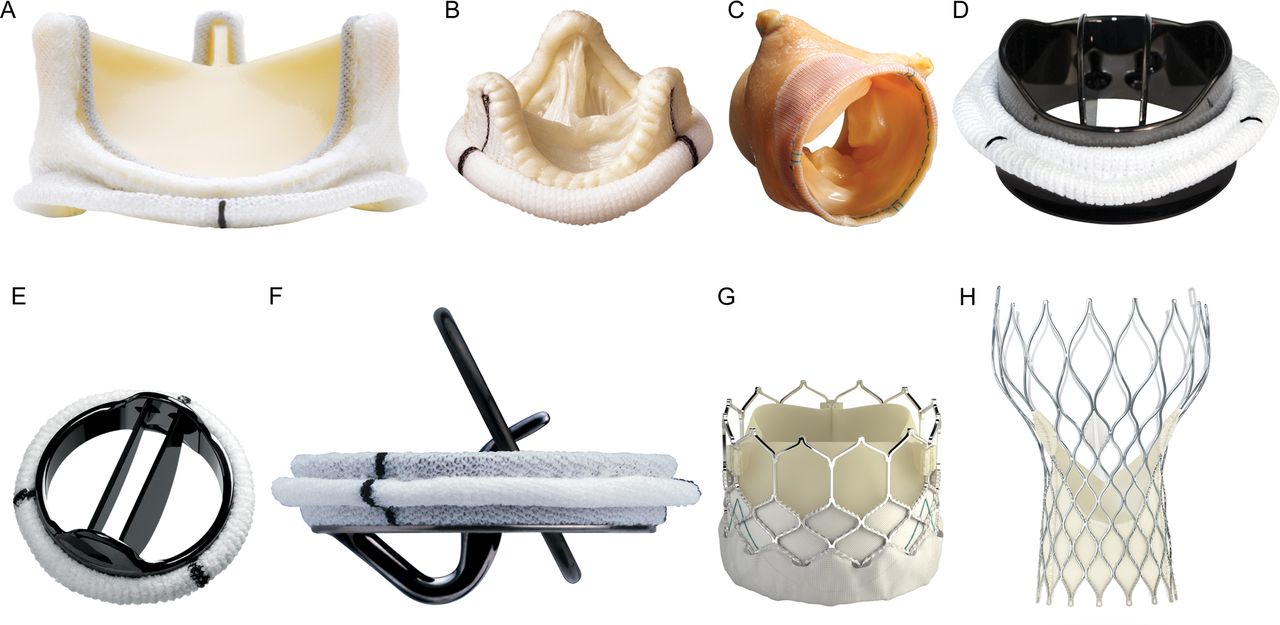
Prosthetic heart valves are available in three broad categories: bioprostonic tissue valves, mechanical heart valves and vascular valves. Bioprostonic tissue valves have the ability to inflate and deflate according to the degree of a heart patient’s disease.
Mechanical heart valves are designed to maintain a constant inflow of blood by exerting a pressure against the diastolic blood pressure and an inflow of blood into the arterial blood vessels. An engineered valve, however, is basically a valve whose inner surface has been carved like a real heart valve. It allows blood to flow continuously into the heart.
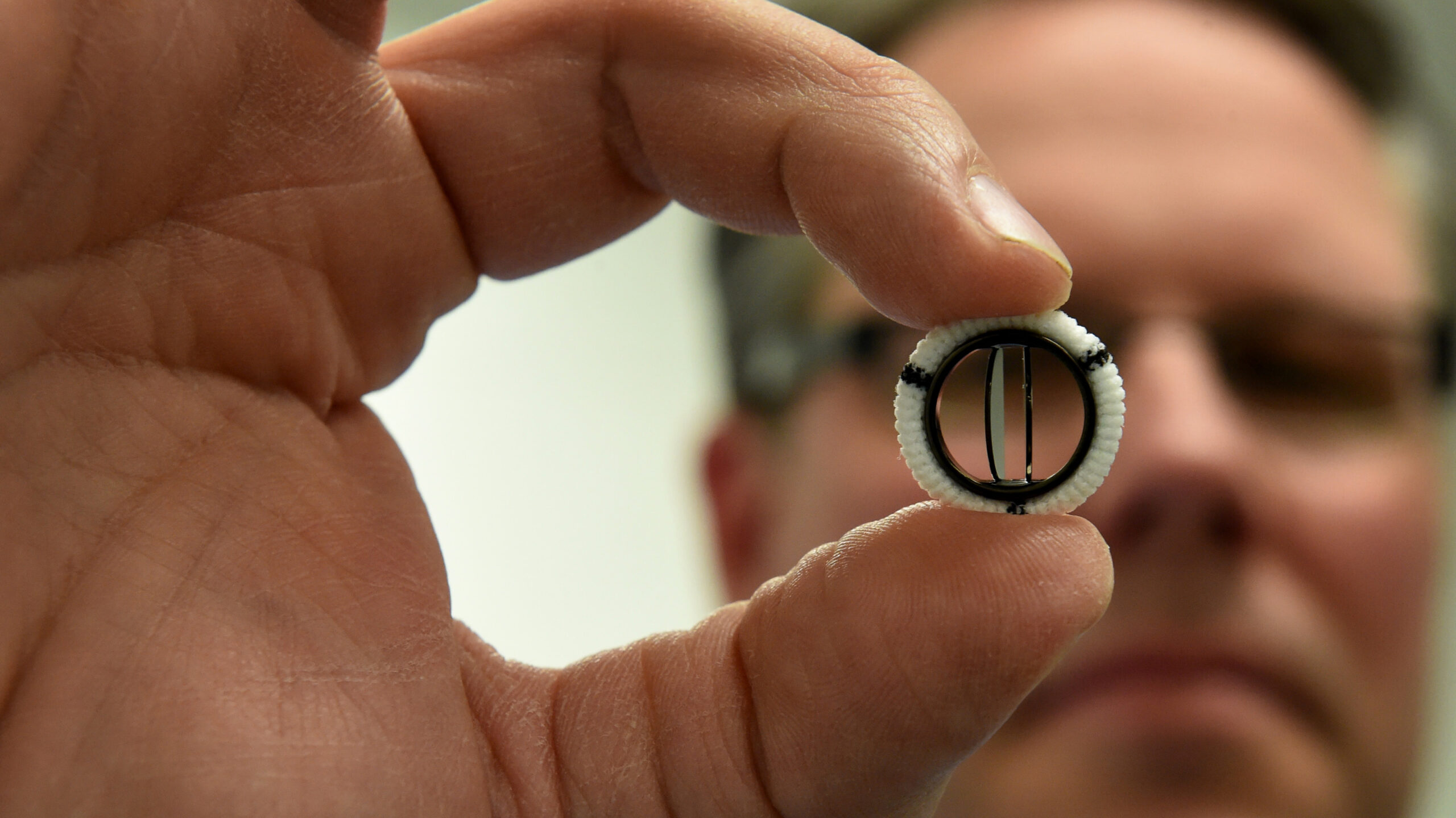
Bio-prosthetics are the type of prosthetic heart valves which are used for patients who have undergone bypass surgery. They are fitted to the inside of the large diaphragm that houses the heart. They have the ability to provide the necessary function to the body. Artificial prosthetic heart valves made from silicon and other materials are called Cardio-vertebral Interface or Mitral Valve Replacement.
The diaphragm is shaped like a donut and is implanted in the cranium. They can either be used alone or in combination with another device such as an artificial diaphragm, stent or stapling. In cardiac surgery, these types of prosthetic heart valves are often used together with stents. Cardio-fracture prosthetic heart valves utilize a combination of silicone and titanium for implantation into the heart.
They are formed as a solid strip that stretches over the entire device. Once secured, they are treated with an elastomeric fluid that forms a protective layer over the device and other components. Since this type of valve is composed entirely of silicone, it has been found to be very durable and reliable, contributing to excellent valve longevity and good tissue construction.
In October 2024, a blood purification solutions providing company in the U.S., CytoSorbents Corporation, completed its REMOVE (Removing Mechanisms and Investigating Efficiency Of Hemoadsorption for Prevention of Vasodilatory Shock in Cardiac Surgery Patients with Infective Endocarditis) study on prosthetic heart valves.
Since the materials used for the construction of the valves are designed to be extremely durable, they will last longer than traditional implantations. Some of the modern materials used in the manufacturing process reduce the number and size of holes that need to be drilled through the rib cage to allow for easy implantation and greater longevity.