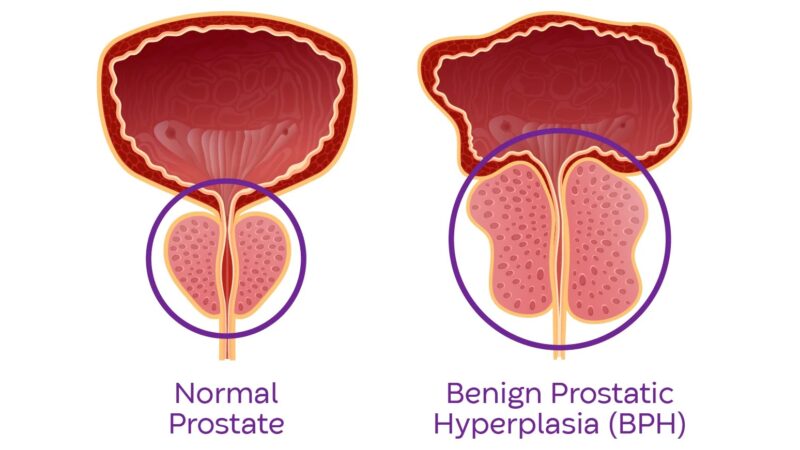
Waking up twice or more each night to urinate disrupts sleep and may indicate benign prostatic hyperplasia (BPH), a non-cancerous enlargement of the prostate gland. The walnut-sized prostate surrounds the urethra just below the bladder, and when enlarged, compresses this tube, affecting urine flow and bladder function.
While prostate enlargement occurs naturally with age, nocturia (nighttime urination) combined with other urinary symptoms often signals the need for medical evaluation.
The International Prostate Symptom Score (IPSS) helps doctors assess severity, with moderate symptoms requiring treatment consideration. Depending on the results, your doctor may recommend lifestyle changes, medication, or specific treatment for enlarged prostate to relieve symptoms and improve quality of life.
Understanding Prostate Enlargement and Nighttime Symptoms

The prostate gland doubles in size between birth and puberty, then doubles again between ages 25 and 50. This growth accelerates after 50, with the transition zone surrounding the urethra expanding most significantly. As prostate tissue increases, it compresses the urethra and pushes against the bladder base, creating two problems: mechanical obstruction and bladder muscle changes.
The bladder compensates for urethral compression by contracting more forcefully, causing the detrusor muscle to thicken. This thickened muscle becomes overactive and less elastic, reducing bladder capacity from a normal 400-500ml to sometimes under 200ml. The overactive bladder contracts before reaching full capacity, triggering sudden urges to urinate.
Nighttime symptoms develop because:
- Horizontal positioning redistributes body fluids, increasing kidney filtration
- Reduced antidiuretic hormone production in older adults increases nighttime urine production
- The enlarged prostate prevents complete bladder emptying, leaving residual urine
- Bladder irritability increases during rest periods
Post-void residual urine—the amount remaining after urination—becomes particularly problematic at night. Normal residual volume measures less than 50ml, but BPH patients often retain more. This retained urine reduces functional bladder capacity, causing more frequent nighttime trips.
Distinguishing BPH from Other Conditions
Several conditions mimic BPH symptoms, requiring careful diagnostic differentiation. Prostate inflammation (prostatitis) causes similar urinary symptoms but typically includes pelvic pain and occurs in younger men. Bacterial prostatitis presents with fever and acute symptoms, while chronic prostatitis develops gradually with intermittent flare-ups.
Bladder stones form when concentrated urine crystallizes, often due to incomplete emptying from BPH. These stones cause sudden flow interruption, blood in urine, and severe pain during urination. Ultrasound can distinguish stones from pure BPH obstruction.
Overactive bladder syndrome occurs independently or alongside BPH. Pure overactive bladder causes urgency and frequency without flow problems. When combined with BPH, patients experience both obstructive symptoms (weak stream, straining) and irritative symptoms (urgency, frequency).
Diabetes affects urination through multiple mechanisms:
- High blood glucose causes osmotic diuresis, increasing urine production
- Diabetic neuropathy damages bladder nerves, affecting sensation and contraction
- Recurrent infections irritate the bladder
Urinary tract infections cause sudden symptom onset with burning, cloudy urine, and sometimes fever. BPH increases infection risk by causing incomplete emptying, but infection symptoms differ from chronic BPH patterns.
Prostate cancer occasionally presents with urinary symptoms, though early-stage cancer typically causes no symptoms. Advanced cancer invading the urethra or bladder neck produces symptoms indistinguishable from BPH without proper testing.
Diagnostic Tests and Evaluation

Digital rectal examination (DRE) allows direct prostate assessment through the rectal wall. The physician evaluates size, consistency, symmetry, and nodules. A normal prostate feels firm like the tip of your nose, while cancer often creates hard, irregular areas. BPH typically produces smooth, symmetrical enlargement.
PSA (prostate-specific antigen) blood testing measures a protein produced by prostate cells. Normal PSA ranges vary by age, with levels generally increasing with advancing age.
PSA density (PSA level divided by prostate volume) helps distinguish BPH from cancer. Higher values suggest increased cancer risk.
Uroflowmetry measures urine flow rate and pattern. Patients urinate into a special toilet that records:
- Maximum flow rate (Qmax)
- Average flow rate
- Voiding time and volume
- Flow curve shape
Post-void residual measurement via ultrasound immediately follows uroflowmetry. Significant residual volumes indicate obstruction requiring treatment consideration.
Transrectal ultrasound provides prostate volume measurement and evaluates internal architecture. The procedure identifies median lobe enlargement, which particularly affects bladder emptying. Prostate volume helps predict medication response and surgical planning.
Urodynamic studies assess bladder pressure and function during filling and emptying. Pressure-flow studies distinguish true obstruction from weak bladder muscle. Higher bladder pressure at maximum flow with lower flow rates confirms obstruction.
Cystoscopy allows direct visualization of the prostate, urethra, and bladder using a thin camera. The procedure identifies strictures, bladder stones, tumors, and the degree of prostatic urethral compression.
Medical Treatment Options

Alpha-blockers relax smooth muscle in the prostate and bladder neck, improving urine flow within days to weeks. These medications don’t shrink the prostate but reduce functional obstruction.
- Tamsulosin (0.4mg daily) selectively targets prostate receptors with minimal blood pressure effects. Side effects include retrograde ejaculation in some patients and occasional dizziness.
- Alfuzosin (10mg daily) provides similar efficacy with potentially fewer ejaculatory problems. The extended-release formulation maintains steady drug levels.
- Silodosin (8mg daily) offers high selectivity for prostate receptors, producing substantial flow improvement but higher retrograde ejaculation rate.
- 5-alpha reductase inhibitors shrink the prostate by blocking testosterone conversion to dihydrotestosterone (DHT). Prostate volume reduces significantly over 6-12 months.
- Finasteride (5mg daily) reduces prostate volume and PSA levels by approximately half. Sexual side effects affect a small percentage of patients and occasionally persist after discontinuation.
- Dutasteride (0.5mg daily) blocks both type 1 and type 2 5-alpha reductase enzymes, potentially providing greater DHT suppression. Both medications reduce progression risk and need for surgery.
Combination therapy using alpha-blockers with 5-alpha reductase inhibitors provides improved symptom improvement for men with larger prostates. Studies have demonstrated combination therapy significantly reduces clinical progression compared to placebo.
Phosphodiesterase-5 inhibitors like tadalafil (5mg daily) improve both urinary symptoms and erectile function. The medication relaxes smooth muscle and increases blood flow in the prostate and bladder.
Anticholinergic medications treat overactive bladder symptoms when combined with alpha-blockers. Solifenacin or mirabegron reduce urgency and frequency without increasing retention risk when obstruction is adequately treated.
Minimally Invasive Procedures

Prostatic urethral lift (UroLift) uses permanent implants to compress obstructing prostate tissue laterally, opening the urethral channel. The procedure preserves sexual function with no reported retrograde ejaculation. Symptom scores improve with effects lasting beyond 5 years in clinical studies.
Water vapor therapy (Rezum) delivers targeted steam to destroy excess prostate tissue. Each 9-second treatment creates a 1-2cm zone of thermal necrosis. The body reabsorbs treated tissue over 3-6 months, reducing prostate volume. Temporary catheterization for 3-7 days manages initial swelling.
Prostatic artery embolization blocks blood flow to the prostate using tiny particles injected through catheter access via the wrist or groin. The prostate shrinks over 3-6 months. The procedure suits patients with bleeding disorders or high surgical risk.
Transurethral microwave thermotherapy (TUMT) heats prostate tissue to 45-60°C while cooling the urethra. The outpatient procedure requires only local anesthesia. Symptom improvement occurs gradually over 3-6 months as treated tissue is reabsorbed.
High-intensity focused ultrasound (HIFU) destroys prostate tissue using focused sound waves. MRI guidance allows targeting while monitoring temperature. The procedure treats specific prostate zones while preserving surrounding structures.
Surgical Interventions

Transurethral resection of the prostate (TURP) is a standard surgical treatment for prostates 30-80 grams. The surgeon removes obstructing tissue using an electrified wire loop through the urethra. Current bipolar TURP reduces bleeding and eliminates TUR syndrome risk from fluid absorption.
The procedure removes tissue, creating a wide channel from bladder to external sphincter. Symptom scores improve significantly, with effects lasting many years. Retrograde ejaculation occurs in most patients, while erectile dysfunction affects some patients.
Holmium laser enucleation (HoLEP) removes the entire transition zone regardless of prostate size. The laser separates adenoma from the surgical capsule, like peeling an orange. A morcellator removes tissue fragments through the bladder.
HoLEP treats large prostates as effectively as smaller glands. Same-day catheter removal and discharge occur in selected patients. Long-term retreatment rates remain low.
GreenLight photoselective vaporization uses a 532nm wavelength laser absorbed by hemoglobin, vaporizing blood-rich prostate tissue. The procedure creates minimal bleeding, suiting patients on anticoagulation. Tissue vaporization leaves no specimen for pathology examination.
Open or robotic simple prostatectomy treats extremely large prostates above 80-100 grams. The surgeon removes the adenoma through a bladder or retropubic incision while preserving the peripheral zone and capsule. Hospital stays average 2-3 days with catheter duration of 5-7 days.
Next Steps
Frequent nighttime urination combined with weak stream or urgency requires prompt evaluation to distinguish BPH from other conditions. Effective treatments range from medications to minimally invasive procedures. Early intervention prevents bladder damage and maintains quality of life.
If you’re experiencing frequent nighttime urination, weak urinary stream, or urgency symptoms, our MOH-accredited urologist can evaluate your prostate and provide appropriate treatment.