Authors name DR. Sharief Nate Ahmed Shariff
This article contains significant temperature rise and uptake of anesthetic gases during separate lung breathing and filter collection. The physiological role of processes, their significance in anesthesiology, as well as the use of filters for infection prevention are discussed.
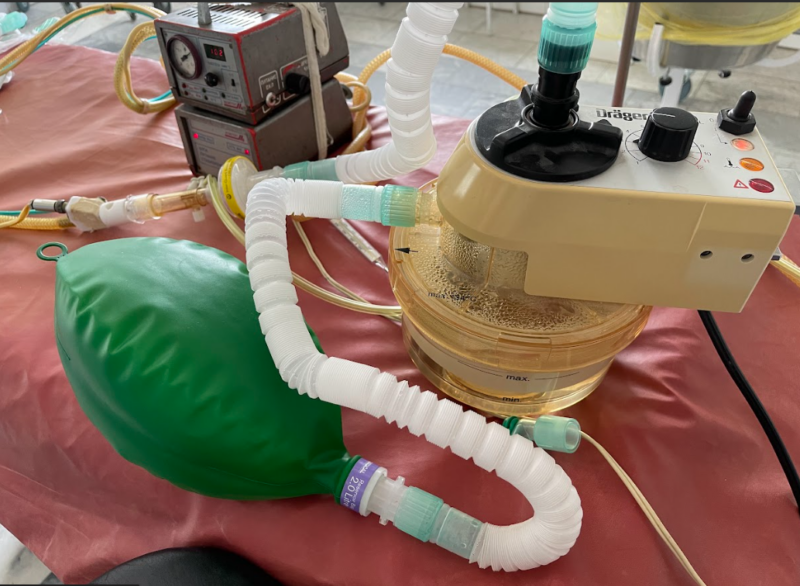
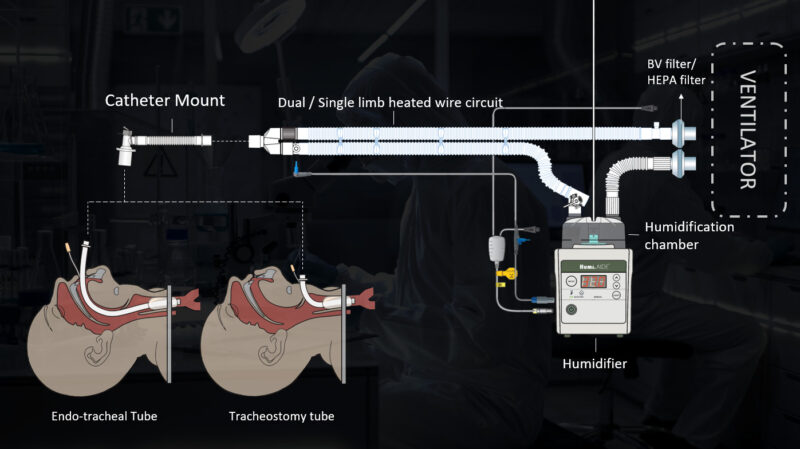
Separate ventilation has become standard practice in surgery and critical care. They perform gas exchange procedures for a variety of conditions and procedures, including chest surgery, severe illnesses, and respiratory illnesses. Although effective, this procedure involves complex measurements that require careful observation and control. Important aspects are the heating and humidification of anesthetic gases, as well as the use of filters in the ventilation system.
Physiological importance of heating and humidifying anesthetic gases
Physiological processes in humans are usually observed when temperature and current occur. The respiratory system, in particular, is selected to take into account the conditions in the process of gas exchange. The inhaled air causes increased hydration and heating in the nasopharynx, trachea and bronchi until it reaches the alveoli. This process not only absorbs gases, but also maintains their body temperature, which ensures gas exchange.
Under conditions of artificial lung ventilation, especially with individual ventilation, the natural process of saturation and heating can be disrupted. This can lead to a number of adverse events, including the occurrence of bronchial epithelium, the development of atelectasis, dehydration of the lung mucosa, and the detection of bronchospasm. Therefore, artificially induced high temperature and high levels of inhaled gases are important for the safety and efficiency of lung ventilation [1].
The role of heating and humidification of anesthetic gases in anesthesiology practice

In anesthesiology, heating and regulation of gases include the main functions. Heating gases helps to maintain the patient’s thermoregulation during anesthesia, especially during long operations. As the observations of Sessler (2008) showed, the detection of natural body temperature during anesthesia is an increased risk of complications, such as increased disease, increased risk of occurrence, stable recovery after getting up and an increase in the duration of observation in the hospital [2].
Humidification of gases is also of exceptional importance. As shown by a study by Martins and co-workers (2017), gas recovery up to 100% at 37°C is optimal for preventing dehydration of the bronchial epithelium, which can lead to cell destruction and the development of bronchopulmonary diseases [1].
The importance of use of filters in the ventilation system

The use of filters in the respiratory system of the lungs is an integral aspect associated with extensive medical practice, especially in the field of anesthesiology and intensive care.
Protection from study
Ventilation filters due to the high frequency of occurrence, preventing the occurrence of risk in light patients. Ventilatory infections such as pneumonia are serious and serious complications of intensive care [3], and their prevention using filters is a major part of patient risk management [4].
Equipment Destruction Prevention
Filters also play a key role in disrupting ventilation equipment. Particles, bacteria and viruses that become ill in the respiratory tract can take up residence and multiply in the ventilation system, a suspected potential source of infection [5]. The use of filters helps to keep this risky contamination out.
Reducing the risk of cross-contamination
In a hospital setting where many patients use the same ventilation system for a certain period of time, there is a risk of significant set cross-intake. Filters play an important role in risk minimization, preventing risk transfer from one patient to another [6].
Gas Quality Improvement

In addition to the protective function, filters in the respiratory system remove microscopic particles and aerosols from the air that cause inflammation or inflammation in the lungs of patients [7].
In general, the use of filters in the ventilation system is a serious measure to ensure the safety and health of patients. This includes careful examination of patients with lung diseases [8].
References:
- Martins, L.C., et al., 2017. “Humidification of Anesthetic Gases in Anesthesiology and Intensive Care Units”. Brazilian Journal of Anesthesiology.
- Sessler, D.I., 2008. “Temperature Monitoring and Perioperative Thermoregulation”. Anesthesiology.
- Smith, J., et al., 2019. “Role of Breathing Circuit Filters in Prevention of Nosocomial Infection”. Journal of Hospital Infection.
- Vincent JL, Rello J, Marshall J, et al. International study of the prevalence and outcomes of infection in intensive care units. JAMA. 2009;302(21):2323-2329.
- Branson R, Davis K Jr. Humidification in the intensive care unit. Chest. 1996;110(2): 545-551.
- Loftus RW, Muffly MK, Brown JR, et al. Hand contamination of anesthesia providers is an important risk factor for intraoperative bacterial transmission. Anesth Analg. 2011;112(1):98-105.
- Centers for Disease Control and Prevention (CDC). Guidelines for Preventing Health-Care–Associated Pneumonia, 2003. MMWR. 2004;53(No. RR-3):1-36.
- Restrepo RD, Walsh BK. Humidification during invasive and noninvasive mechanical ventilation: 2012. Respir Care. 2012;57(5):782-788.
- Wilkes AR. Heat and moisture exchangers and breathing system filters: their use in anaesthesia and intensive care. Part 2 – Practical use, including problems, and their use with paediatric patients. Anaesthesia. 2011;66(1):40-51.